Corvallis Birth & Wellness Center offers specialized gynecology and pelvic health services for issues such as:
- pelvic pain
- vaginal pain
- pain with intercourse
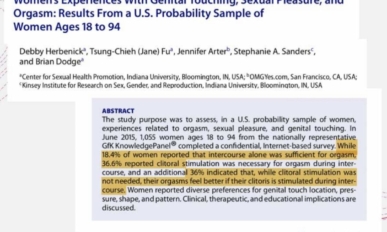
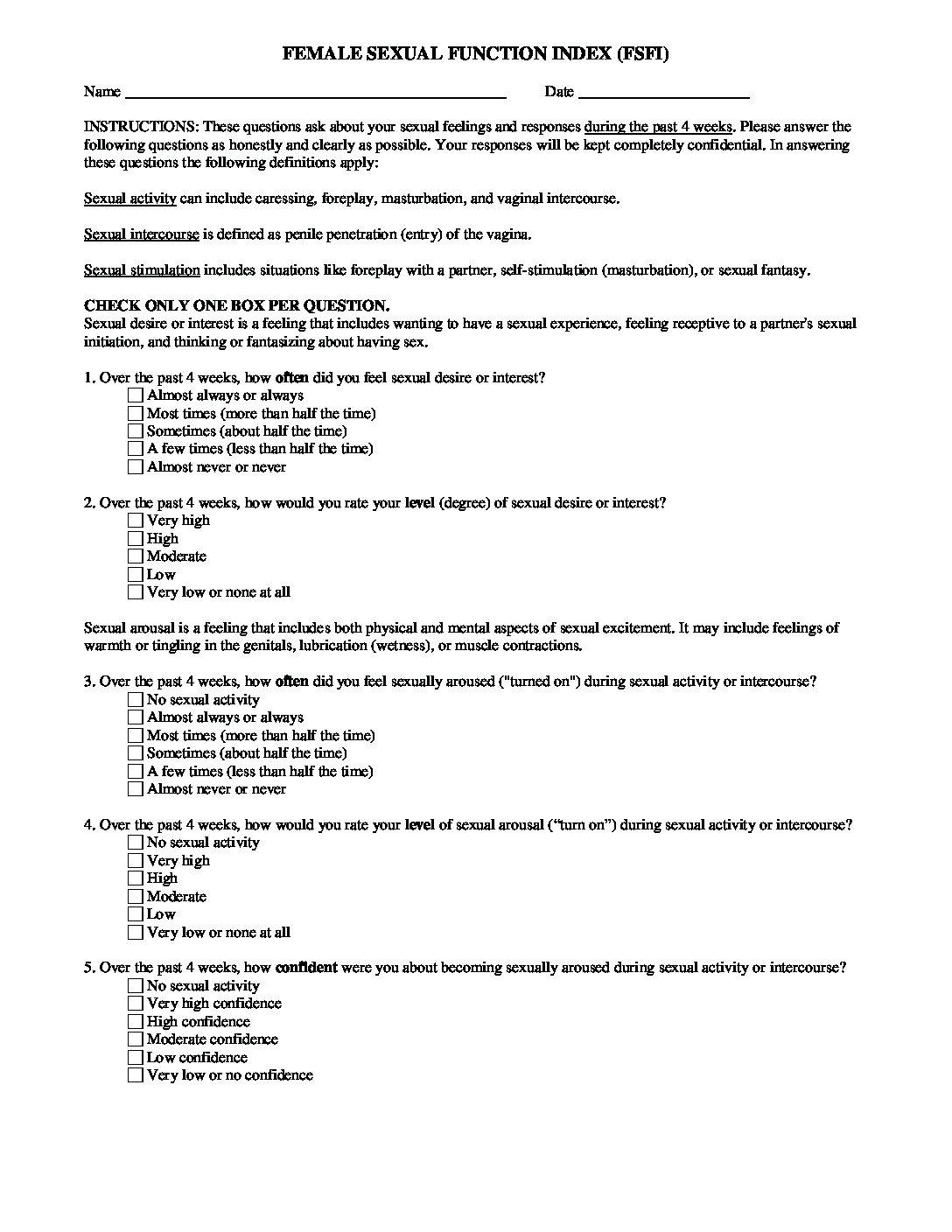
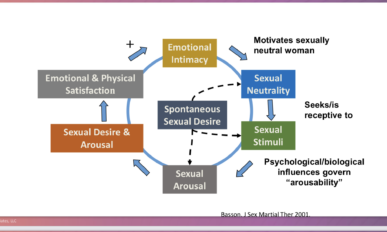
- sexual concerns
- incontinence
- Genitourinary Syndrome of Menopause (once known as atrophic vaginitis)
- Menopausal changes and hormones
Susan Heinz, DNP, CNM is focusing much of her practice on working with individuals with issues around pelvic pain and pelvic relaxation, and menopausal changes. She offers therapies such as mayan abdominal therapy and myofascial release, trigger point release, and biofeedback. Hormonal treatment and alternative treatments for decreased sex drive, vulvar and vaginal pain, and genitourinary syndrome of menopause, and menopausal changes.